Impact Analysis of Proposed Changes to ACA Medicaid Expansion Funding
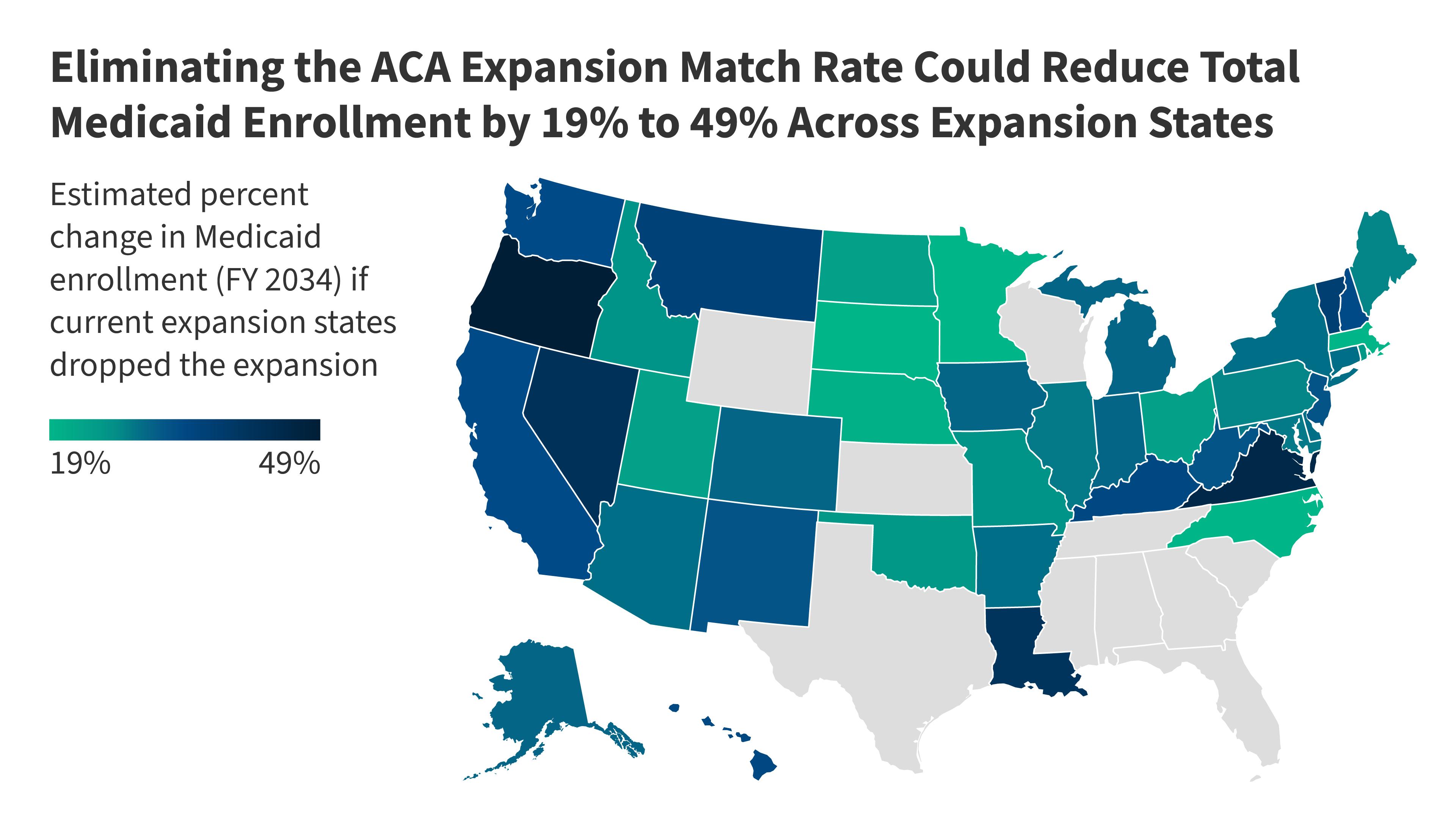
Examining the potential effects of a proposal to eliminate the 90% federal match rate for the Medicaid expansion under the Affordable Care Act (ACA) reveals significant consequences for states and enrollees. Currently, this expansion covers more than 20 million individuals.
Key Insights:
-
Continued State Coverage: Should states decide to keep coverage intact, federal Medicaid funding would drop by $626 billion, while states would see their spending increase by the same amount over the next decade.
-
Scenario of Dropping Expansion: In an alternate scenario where states choose to discontinue the expansion, federal spending would plummet by $1.7 trillion, and state expenses would decrease by $186 billion. This would lead to approximately 20 million people losing their coverage.
This policy adjustment has the most profound effect on states that have previously adopted Medicaid expansion. The analysis also explores the possible ramifications for states with Medicaid expansion trigger laws and how reduced federal support might influence both coverage and health outcomes.